This morning’s Chron is full of delights. Not only is Mayor Breed moving to make the marvelous restaurant parklets permanent, but our county is expanding its vaccination protocols to include several important populations, amongst which is our jail population! Aidin Vaziri reported:
The city will also open appointments to individuals who live or work in high-risk congregate care settings, including correctional facilities, homeless shelters and residential care and treatment facilities, the Department of Public Health announced Friday. People experiencing homelessness will also be eligible.
“Getting vaccinations to people with disabilities and who have severe underlying conditions, and people who are in congregate settings, is an important part of our efforts to save lives and protect our most vulnerable residents,” Mayor London Breed said in a statement.
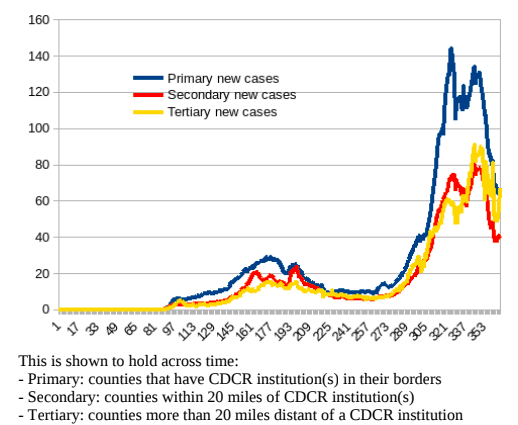
This is a key move for the various reasons I explained in my previous post and in my new article. Other counties must follow San Francisco’s lead, and if they don’t, a state mandate must be put in place so that jail populations, which are transient by their very nature and a crucial juncture in the community-to-prison-to-community multidirectional pipeline, do not act as superspreading disease points. Here is what I wrote about vaccinating jail populations:
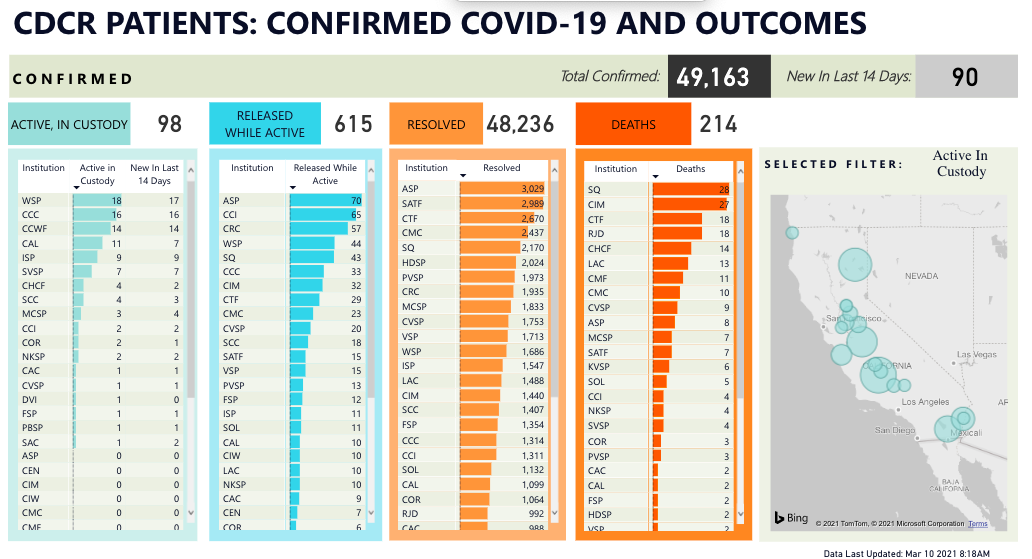
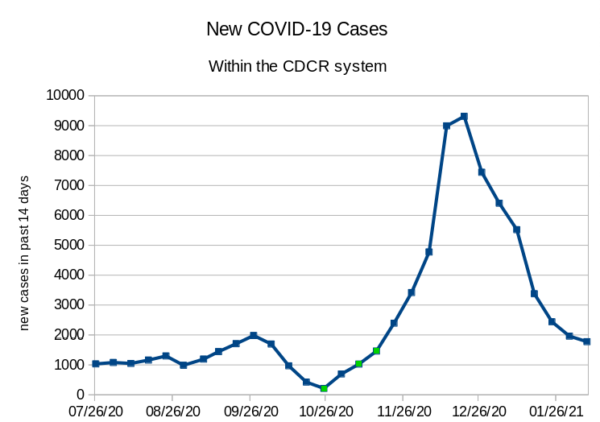
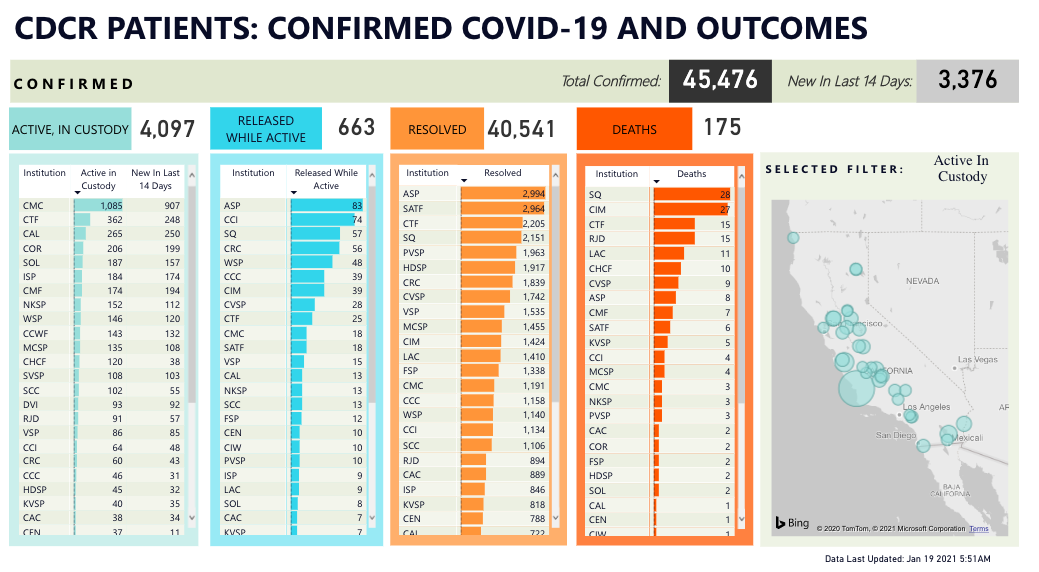
The advent of the Pfizer and Moderna vaccines opened a new avenue of advocacy on behalf of incarcerated populations. Given the prioritization of vaccinating people in congregate housing settings, such as nursery homes, similar arguments were made in the context of prisons. The same arguments can, and should, be made on behalf of residents of county jails. In California, the concerted effort of advocates and experts led to the classification of people in prison as vaccine priorities, in Tier 1B; despite a disappointing January retraction of this policy, as of February 23, 2021, 40 percent of the prison population has been vaccinated. Despite understandable concerns that incarcerated people might harbor mistrust and suspicion of prison authorities, which would stand in the way of administering the vaccine, the acceptance rate among incarcerated people has been high; refusal rates have only been problematic among the staff.
It is here where, once again, the jurisdictional-mechanistic approach to county jails works to the detriment not only of their residents, but of all residents of the surrounding and neighboring counties: Even before it was rescinded, the California state mandate extends only to state prisons. Counties were left to decide for themselves whether to prioritize their jail populations and, as in other matters, there has been considerable variation. Bay Area counties are ramping up vaccination for their jail populations; Kings and Tulare counties are vaccinating aging and infirm jail residents, while Merced and Fresno Counties have no set date yet to begin vaccination in their jails.
While these variations in vaccine policies could be simply manifestations of supply shortages, they might also represent political pushback in the counties of the sort seen in other states regarding prisons. In Colorado, for example, Governor Jared Polis responded to public pressure by ignoring expert opinions on the urgency of vaccinating incarcerated people for public health and downgraded this population in his plan. The Director of the Center for Bioethics and Humanities at the University of Colorado criticized this decision as guided by “moralistic argument,” explaining that “[i]t’s a very stigmatized population, and there are people who say, ‘They’re in prison, they must have done something terrible, and they don’t deserve a place in line.’”
The prevalence of such “moralistic arguments,” which compound public health priorities with hierarchies of perceived deservedness, might play into the struggle for vaccination in jails. As explained above, 75% of the California jail population consists of pretrial detainees who, of course, are presumed innocent; it is not difficult to imagine an appeal to public policy that distinguishes between these people and the presumably “less deserving” people in state prisons.
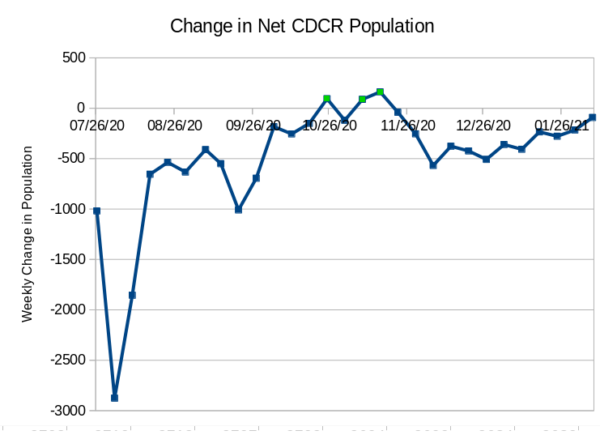
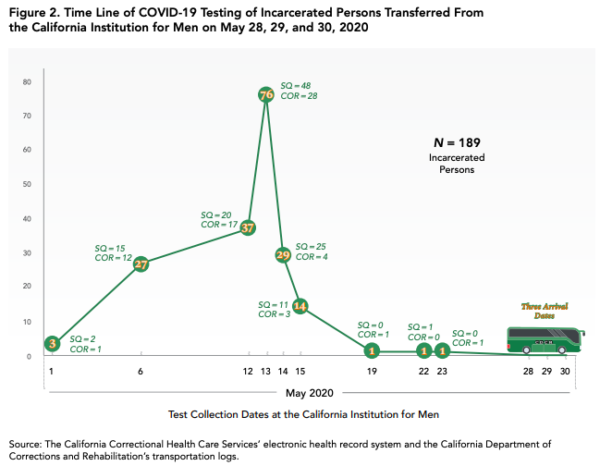
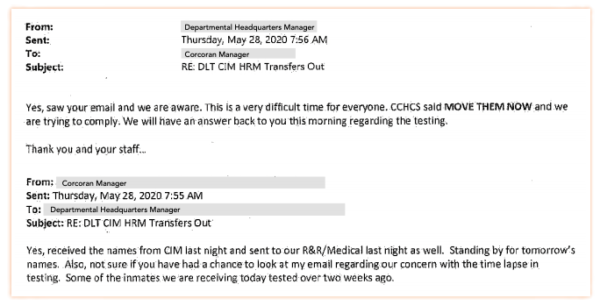
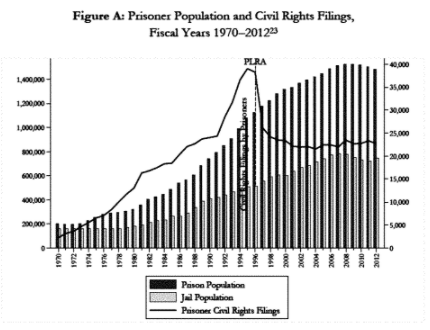
Despite its superficial rhetorical appeal, I strongly advise against relying on such an argument. Adopting the organic-geographical perspective that this article proposes implies seeing all incarcerated people in California as part of one porous carceral network, along a continuum that reaches to the outside community. The bottleneck effects of the jurisdictional approach have led to outbreaks; the way out of this quagmire requires accepting the need for population equilibrium and population reductions throughout the entire correctional system, regardless of administration and budgeting levels. Part and parcel of this essential population reduction is opening the jail floodgates, not only through releases to the population, but also as a two-way flow to and from the prisons. Under such circumstances, it is unacceptable to continue mixing vaccinated and unvaccinated populations. Moreover, 25% of the jail population consists of sentenced individuals, many of them for felonies; taking the deservedness argument to its conclusion would lead to the absurd policy of vaccinating only some jail residents and leaving others exposed. Such a policy would be impossible to justify and would have unbearable equity and public health implications.
Instead, I propose advocating the vaccination of the jail population by relying on two arguments with organic-geographical appeal. First, it must be clear that the transient jail population poses at least as much risk to the surrounding community as the staff working among the less transient prison population. The reasoning for vaccination in both cases should be the same. In addition, there is a practical consideration that should appeal to counties and municipalities: running a vaccination enterprise at a congregate housing location with permanent medical staff would ease vaccine distribution, help with the dissemination of medical information, and possibly have the ripple effect of generating more vaccine acceptance among family members and friends of people who are vaccinated during the course of their jail residency.
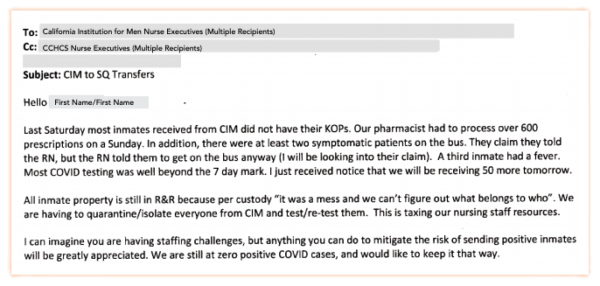
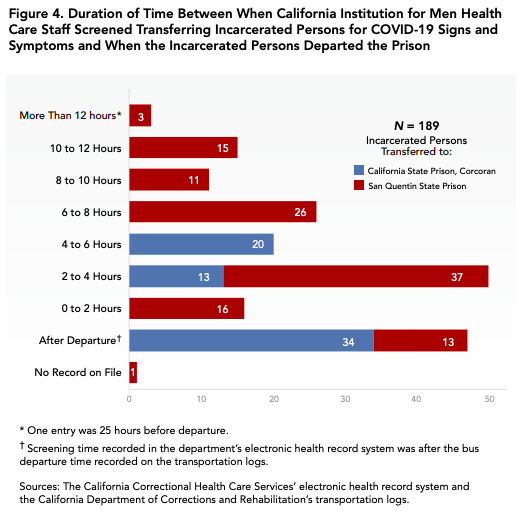
While the project of vaccinating incarcerated populations is worthwhile, it raises the concern that the vaccine would come to be seen as the panacea for all correctional problems. This article’s review of the spillover of healthcare problems from prisons into jails should be a cautionary tale.
My recommendations for remedying the broken healthcare structure in county jails require a paradigm change, which would view jails not through the jurisdictional-mechanistic perspective, but as organic parts of their surroundings and communities. Unifying the administration of prisons and jails in California might be a pipe dream; however, at bare minimum, health care policies should be far better coordinated. Informational databases—not only involving healthcare, but also population shifts—should have seamless interfaces between state and county facilities (an inexcusable oversight in a state with such high technological literacy.) Aggressive efforts at hiring and retaining medical staff should target not only individual facilities, but also local county hospitals with an eye toward serving incarcerated populations as well. Most importantly, health care policies, ranging from preventative healthcare, nutrition and wellness, to emergency care, should start with families and schools, extending into jails and prisons as a continuum. These are crucial not only to curb the current pandemic, but also to prevent the pandemics of the future.