As regular followers of the blog probably recall, the CA Supreme Court ordered to remand Von Staich to the Marin Superior Court, where Judge Geoffrey Howard will be presiding over an evidentiary hearing. The hearing is scheduled to begin this coming Thursday at 9am, via Zoom.
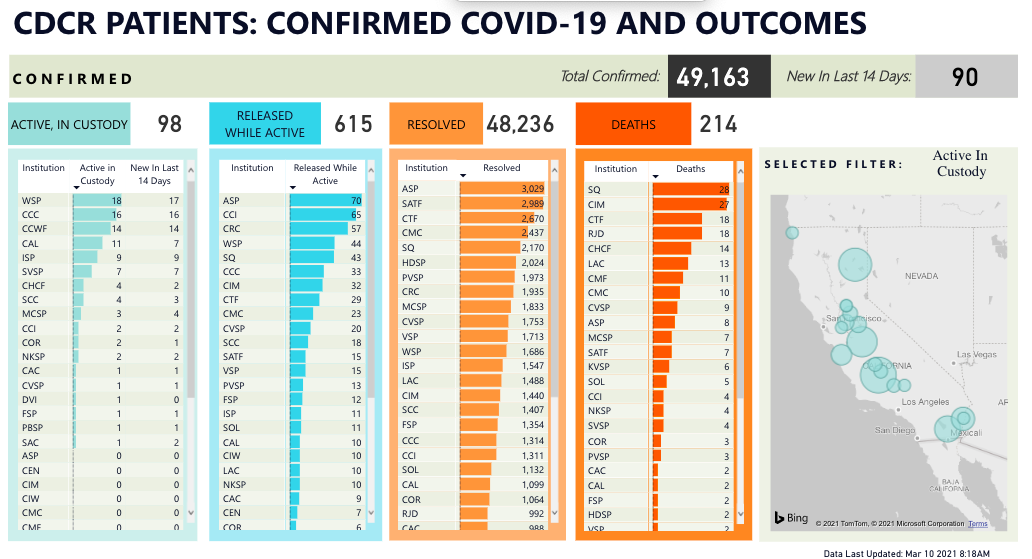
The factual question the court must resolve is whether CDCR acted with deliberate indifference by failing to protect the health and safety of petitioners, who are several hundred members of the San Quentin prison population. The Petitioner’s lawyers–some of them from private law firms, some of them from the Public Defender’s Office, some of them from the First District Appellate Project–will lay out the evidence of the devastation at San Quentin, which ailed thousands of people (more than 75% of the prison population) and killed 28 prisoners and one staff member. An important focal point of the hearing will likely be the OIG’s scathing report from February 1, which details the gross mishandling of the CIM transfer into Quentin (including email screenshots.) There will also be evidence of the lived experience behind bars, which will come from currently and formerly incarcerated witnesses. Given the obvious magnitude of the disaster, it is likely that the Attorney General representatives, who are arguing for CDCR, will focus on the ameliorative steps they took in the aftermath (masks? posters?) and argue that the cumulative effect of their behavior in the crisis falls short of the deliberate indifference standard. They are also likely to argue that, when the contagion broke at Quentin, we knew a lot less than we know now about ventilation (compare to this much newer report by AMEND about conditions at SATF) and that it is unfair to judge their mishandling of the crisis in hindsight.
The last two days featured case management conferences, in which Judge Howard has tried to encourage the parties to cull their presentations so that the hearings can proceed in a timely manner. Part of me wishes that the whole thing were televised, so as to keep a record of what happened in the prison (we will provide such a record in Chapter 3 of #FESTER.) But the hearing is not purely ceremonial–it has real import to real lives in real time–and so, it has to be conducted efficiently.
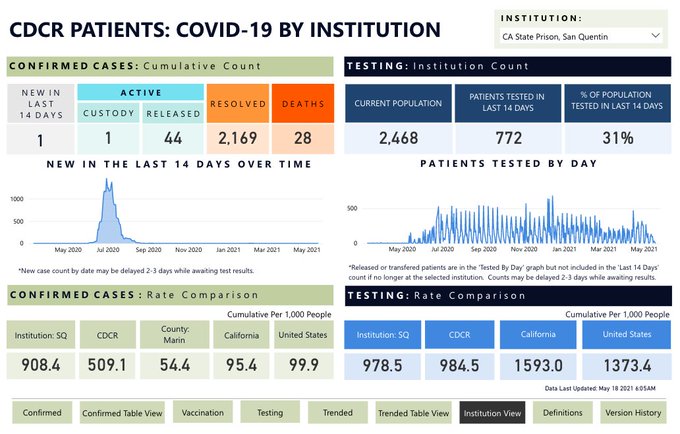
The first difficulty is that some of petitioners’ witnesses are currently incarcerated. This raises logistical challenges because, apparently, it is complicated to set up functional Zoom rooms in prison, and because West Block is currently under lockdown. The Quentin COVID numbers for today (above) do not betray the cause of this, as there is only one active case, but our records reveal two more cases a couple of weeks ago, so it makes sense that a prison wing is quarantined. In addition, I’m sure petitioners are concerned about retaliation against the witnesses, which adds stress (but also gravitas) to the testimony of those who are going forward. There was some debate today about hesitancy to testify, and the AG representative reminded that witnesses must testify. I trust the judgment of the petitioners’ lawyers in this matter.
The second issue is time. The hearing begins on Thursday and the parties have to prep for that as well as continue negotiating factual stipulations and culling the list of witnesses.
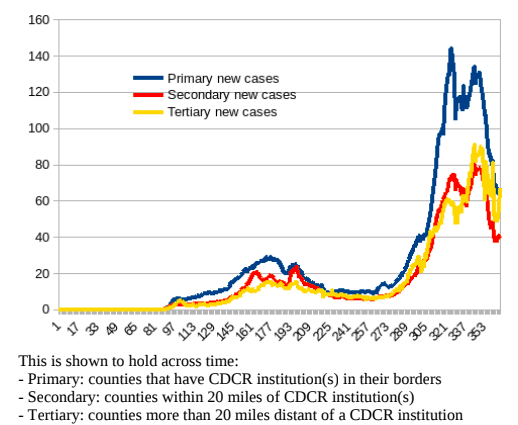
But the most serious issue, which was left unspoken at today’s hearing, is the remedy. As you’ll recall, the original Von Staich decision ordered San Quentin to reduce its population to 50% capacity, but it did not specify how to do so, which led CDCR to opt for transfers rather than releases. Even at that point in the pandemic story, this was akin to playing Tetris with human lives. The outbreak in Quentin was quelling while case numbers at the facilities targeted for transfers were climbing (remember the horrible numbers at Avenal, SATF, CMC, and elsewhere in November/December?) Not only would it be an enormous risk to transfer people to facilities that were in worse shape, but this would also awaken all kinds of inter-facility animosities; I received numerous letters from prison in which people told me that they feared retaliation from people in other institutions for all kinds of historical conflicts and beefs.
These factors are still significant today, but there are a few additional ones. The population at Quentin tends to be older and serve longer sentences, which means a lot of the people who end up at Quentin are in the process of preparing for parole and resentencing hearings, and to do so, they must rack up rehabilitative programs and chronos (laudatory write-ups) for their dossier. Quentin has a wealth of programming that is unavailable in other facilities (no thanks to CDCR; thanks to the many Bay Area do-gooders who volunteer in prisons.) Shifting people between prisons when there is no medical reason to do so–and there hasn’t been in months–is going to sabotage these releases and ultimately cost more, in terms of health risk and money, than no remedy at all. The only worthwhile remedy to consider would be releases, which has been an uphill battle all along, but which are essential to prevent not only a recurrence of COVID (note that there’s a steady stream of transfers from jails, to the tune of hundreds of people every week,, and that the vaccine uptake rate in jails is abysmal) but also future pandemics.
In short, this is in some important ways not unlike the financial considerations I discussed in Cheap on Crime: We simply cannot afford to lock that many people up, because it is impossible to provide them minimal guarantees of health and safety under these conditions.
I will cover the evidentiary hearing with great interest and concern in my next posts. Tune in tomorrow for new information on vaccination in jails, complete with a review of the lousy, low-quality data obtained from sheriffs, courtesy of the excellent Aparna Komarla of the Davis Vanguard‘s superb project COVID-19 in California Jails and Prisons.