The Scorpion and the Frog
The results of the election did not bring me immediate solace. I’m sure this has been the case for many folks who found it difficult to take off the psychological backpack we have been carrying for so long. In my case, the psychological weight is the product of daily engagement with this administration on various public forums, including having to spend least thrice a week, WEEKLY, for the last four years, in TV stations and radio studios talking about this. In November 2016, when I lost the fight for death penalty abolition and my beloved cat Spade on the week of the election, I made it my mission to be an expert in everything these cartoon villains were cooking up, and every morning I sat up abruptly in my bed, with my first thought being, “it’s already morning in D.C., what has he done today?” Every time I saw an unrecognized number on my phone it was a TV producer or journalist asking me things that I had to cram on. I’ve crawled through information on abominable, underhanded things that I could not have even imagined possible before the last four years. Engaging with this sewer of an administration every day, including weekends, has brought exhaustion and stress into our family life, soured my good humor and my patience at work, and taken a real, measurable toll on my health. Doing upbeat explainers, volunteering, and taking abuse via phone and text from voters has felt like wading through a swamp, and even though I wore my psychological hip waders, I resent and revile this administration for demanding that I set aside my own grief, decency, and decorum, and be constantly on-call to respond to venal, opportunistic excrement. After I gave the explainer on Justice Ginsburg’s replacement process, I could barely get out of bed for a few days.
But the miasma in my soul is slowly dissipating. The first time I felt truly rapturous was when I got a letter from Traci Felt Love, the organizer of Lawyers for Good Government. The letter reminded me of when we started L4GG and brought back the incredible week in which we shut down San Francisco International Airport in reaction to the Muslim ban. It was only then that the magnitude of our success in dethroning this monster started to hit me, and I’ve been slowly digesting it.
One thing that has greatly helped is ignoring the legal pageant of the absurd that Trump is mounting in various courts around the country. I have given myself permission to disengage from all his frivolous lawsuits, antics, last-minute personnel juggling, and desperate cries for attention. In January, no matter what happens in the interim, Joe Biden will be President of the United States. Whether Trump concedes (ya think?), resigns (hmmmm), flees to the Cayman Islands to a mansion with golden toilets (on brand) or is dragged out of the White House in handcuffs (appealing but dangerous), the outcome will be a change in administrations.
It’s useful to keep in mind the story of the scorpion and the frog. A scorpion, which cannot swim, asks a frog to carry it across a river on the frog’s back. The frog hesitates, afraid of being stung by the scorpion, but the scorpion assures the frog he won’t do that: “If I sting you, we’ll both drown, right?” This argument convinces the frog, which agrees to transport the scorpion. Midway across the river, the scorpion stings the frog anyway, dooming them both. The dying frog asks the scorpion why it stung despite knowing the consequence, to which the scorpion replies: “I couldn’t help it. It’s in my nature.”
Trumps are going to Trump. Giulianis are going to Giuliani. McConnells are going to McConnell, with or without us as their audience. It’s far more productive to focus our attention on the upcoming races in Georgia.
Drug Truce
Throughout the country, drug law reform gained more momentum. This wonderful post on the Drug Policy Alliance blog summarizes some of the main reforms, the most impressive of which was Oregon’s approval of Measure 110. The next step in procuring a truce on drugs was always going to be branching beyond marijuana, and for various political reasons that are difficult to explain to people outside California, I expected another state to move in that direction first.
What I find especially thrilling about the passage of Measure 110 is that it could open the door to an important dialogue about the value and benefits of psychedelics. MAPS has been leading the charge on declassifying these important substances and acknowledging their potential to help people with depression and trauma, as well as foster spiritual growth. Little by little, the hypocrisy is dissipating, but it’s going to happen on the state and local level first.
When the Perfect Is the Enemy of the Good
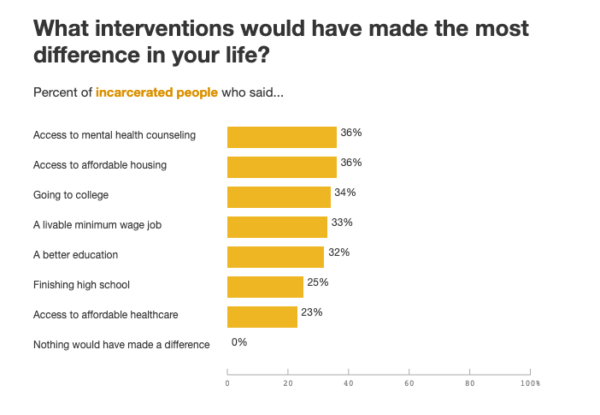
Amidst my joy about the passage of Prop 17 and the failure of Prop 20–a reactionary law-and-order package–the demise of Prop. 25 brought me some anguish. As I explained elsewhere, all the arguments against the abolition of cash bail were ridiculous except for one, which had superficial appeal: the idea that “algorithms are racist” and that we would end up with “something worse” than cash bail. Aside from the fact that it’s hard to imagine how risk assessment is “worse” than debtor prisons straight out of a Charles Dickens novel, there’s a basic misunderstanding of how algorithms work. I have been explaining and explaining, but for some reason am not getting through to people captivated by woke rhetoric: ALGORITHMS ARE NOT RACIST. They predict the future on the basis of the past. If they have racially disparate outcomes, it’s because they reflect a racist reality in which, for a variety of systemic, sad, and infuriating reasons, people who are treated like second-class citizens in their own country commit more violent crime. The overrepresentation of people of color in homicide offenses and other violent crime categories is not something that progressives like to talk about, but it is unfortunately true–not just a mirage caused by stop-and-frisk in low-income communities. The reasons why more African American people commit more homicides than white people are the same reasons why they are arrested more frequently for the drug offenses they don’t actually commit more than white people: deprivation, neglect, lack of opportunities, dehumanization and marginalization on a daily basis. Solving these problems requires an administration committed to treating its citizenry fairly, not sweeping them under the rug by ignoring predictive tools that show what is actually going on. So powerful is the progressive self-deception that the ACLU, initially a supporter of eliminating cash bail, opted not to have a position on the ballot, because of the optics. I can’t even begin to tell you how many people I like and respect opposed Prop 25 using organizations’ positions as proxy, as if they couldn’t think for themselves. These organizations’ and people’s fears of being perceived as racists by supporting “algorithms,” the bogeymen of the left, was so overpowering that it hijacked the very real possibility to get rid of an actual, real, on-the-ground, in-the-open perversity: the only-in-America notion that people should pay money for their pretrial release.
The counterargument, made by some thoughtful folks, was that rejecting Prop. 25 would lead to a better proposal to abolish cash bail. But this argument exhibits deep ignorance of how political gains are made. Part of why I’m so upset about this is that I’ve already lived through a horrible round of the Perfect-Is-the-Enemy-of-the-Good game. Back in 2016, when we campaigned for death penalty abolition, I had to respond to arguments by progressives who thought that abolishing the death penalty was going to somehow “retrench” life without parole. The preciousness of this view infuriates me. As I explained until I was blue in the face, political progress is made incrementally. You can’t get to LWOP abolition without death penalty abolition. Expecting ballot propositions, which have to rely on broad coalitions, to be tailor-made to one’s exquisitely purist views about the public good is a recipe for disappointment. And, as Gov. Newsom said, the demise of Prop 25 essentially eliminates any possibility, motivation, or energy for getting together the “more perfect” solution to the bail problem that activists are yearning for. So, instead of celebrating the end of cash bail, progressives have yet again been duped into failing their own cause because the compromise wasn’t photogenic enough for them, and the big winner has been the bail bonds industry–you can see in this piece how effectively these scoundrels have coopted wokespeak to keep Victorian debt prisons alive.
Got a Sane Idea? Great! Wrap It in Sane Packaging
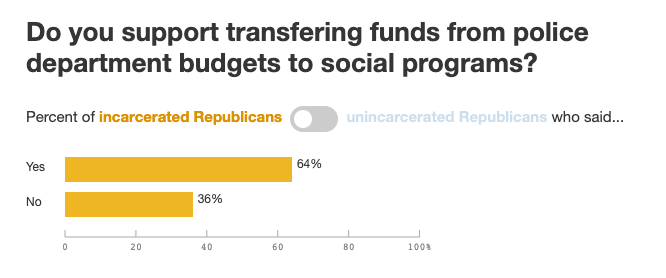
Just read a terrific Mother Jones article, which highlights the success of various local initiatives to divert resources from policing to less confrontational alternatives. Beyond my satisfaction with this outcome, I’m pleased with the rhetorical strategy used in these initiatives.
In the aftermath of the killing of George Floyd, many advocates were making proposals that sounded scary, because they were wrapped in odious movement jargon (defund! abolish! dismantle!). Thing is, the proposals themselves were not radical or insane; they were sane enough that even people who were victimized in scary ways could see the logic in them–if they had the background to understand them. Alternatives to policing are not earth-shattering discoveries. Anyone, not just hyperprogressives, who walks around the Tenderloin these days can sense the palpable shift in energy since the arrival of the wise and conciliatory Urban Alchemy folks. All these propositions are doing is rolling back the Nixonian logic, according to which you somehow get more justice if there are more cops, riot gear, and weapons on the streets. We were sucked into this insanity in the 1970s with the LEAA funding scheme, and later in the 1980s with civil asset forfeiture. You could be forgiven for thinking that “defunding the police” is an extreme proposal if you’re not familiar with how police departments used to be run before they became bloated paramilitary organizations.
But the success of this measures was not only rooted in their inherent reasonableness (and cost-effectiveness.) It was rooted in wise, matter-of-factly packaging, which offered positive alternatives to policing that people could get behind. There is an important lesson here for progressives looking for referendum victories, which I very much hope will be learned: packaging matters. Offering people a realistic vision of humane, therapeutic, preventative public safety works better than wrapping sane, totally plausible ideas in flurries of self-righteous performativity. And that means resisting the cultural zeitgeist, which pushes the movement to flood social media with the most preposterous, off-putting jargon, even when proposing things that would appeal to a broad swath of the population.
When incendiary terminology is used to explain sane, effective reform, more time is spent debating the terminology and performatively defending it than discussing the policies themselves. People who are put off by the rhetoric are exhorted to “check the website,” “do the work,” and “educate themselves” by folks who do not inspire any desire to engage any further with them or with their ideas. Indeed, one of the dumbest aphorisms of this movement is the classic “it’s not my job to educate you.” It’s nobody’s job to educate anyone else (except, in the case of teachers, their actual students.) But hurling insults and disdain on people, piling nonrequired homework on their backs, hiding good ideas behind performative nonsense, and finding fault in people asking to know what they’re expected to support and vote for, is not particularly likely to induce them to take the trouble to learn somewhere else. Decrying the burden of “unpaid emotional labor,” another unfortunate classic, is also not particularly persuasive. Not everyone needs to dance through their revolution like Emma Goldman, but very few people want to get flogged through it. Corollary: If you call yourself an activist, and you want to bring people to your coalition, yes, it is part of your job to educate them. I’m so pleased that the advocacy for these proposals took a different approach, one that voters could get behind. The result will be safer and happier streets in many U.S. cities.